Having diabetes puts you at risk for several possible complications including vision loss that can progress to blindness and foot damage that might lead to amputation. If you have diabetes, this may sound frightening, but there are steps you can take to reduce your risks and tools that can help you manage these complications.
Table of Contents
Vision Loss in People with Diabetes
Why does diabetes cause vision loss?
Types of Eye Problems
When to Call a Doctor
How to Manage Vision Loss or Blindness
Foot Problems
Why does diabetes cause foot problems?
When to Call a Doctor
Prevention
Vision Loss in People with Diabetes
Why does diabetes cause vision loss?
If your blood glucose (sugar) levels are too high for too long, it can damage your eyes. Controlling your glucose levels is important because diabetes is the primary cause of blindness in adults 20-74 years old. With proper management and care, including consulting with your doctor, many eye conditions can be prevented, delayed, or treated.
Types of Eye Problems
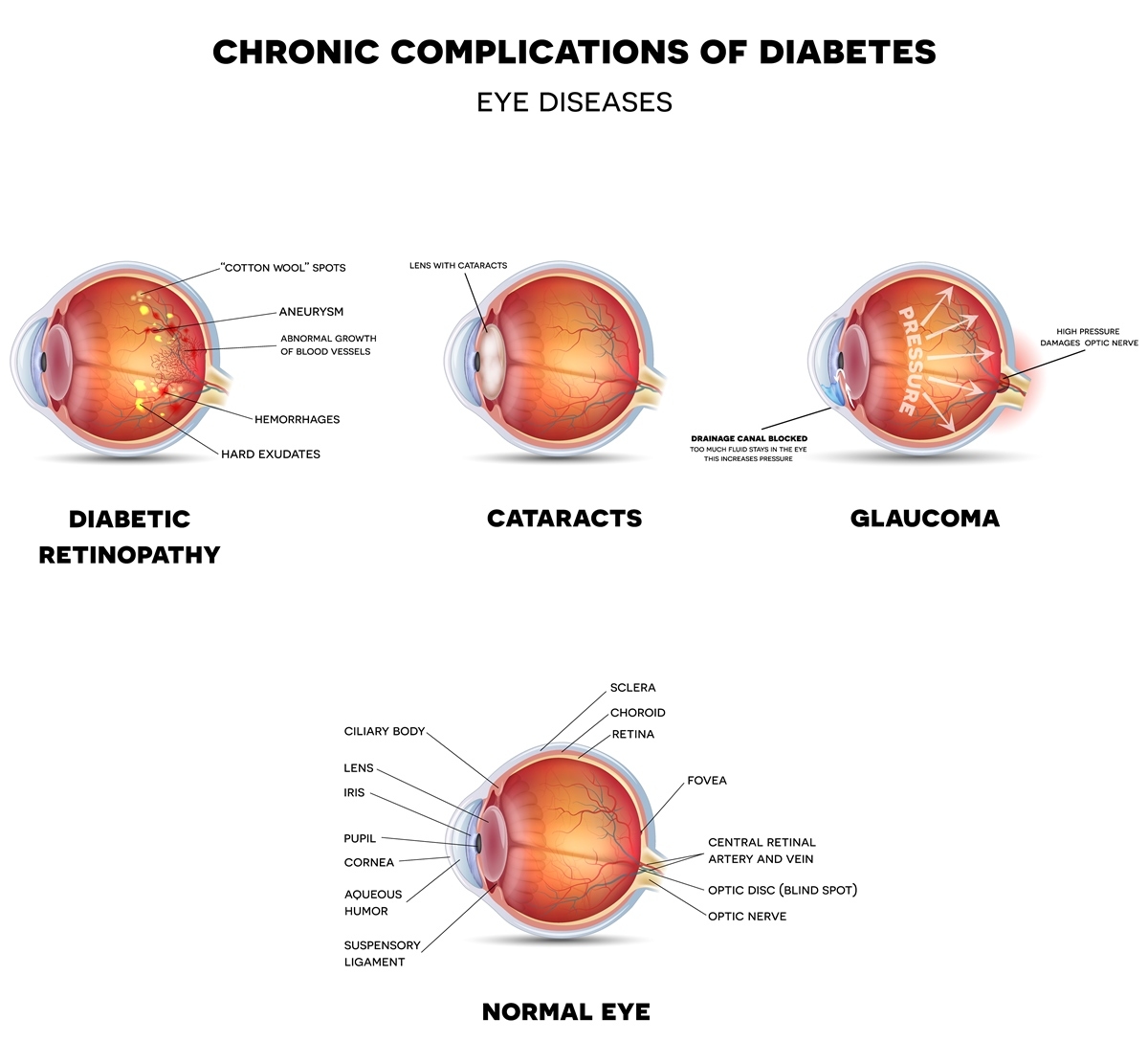
- Diabetic Retinopathy
- The most common eye problem for people with diabetes
- Damage to blood vessels in your retina (back of your eye) due to high blood sugar can eventually lead to blindness
- Symptoms: Blurry or double vision, eye pain and pressure, dark spots in your vision, blank spots, flashes, or rings, and loss of peripheral vision
- Treatment: The sooner it’s caught, the more options you'll have, so talk to your doctor right away
- Blurry Vision
- This can occur due to high blood sugar that makes your lens swell
- Treatment: Getting your glucose back into target range to fix the problem can take up to six months
- Contact your doctor to see if the problem is more serious
- Cataracts
- You are two to five times more likely to develop cataracts if you have diabetes
- A cloudy covering over your lens that prevents your eye from focusing
- Symptoms: Blurred vision and glare
- Treatment: A surgeon will need to replace your lens with a artificial one
- Glaucoma
- Diabetes nearly doubles your risk of glaucoma
- A build up of pressure when fluid is trapped inside your eye
- Symptoms: Headache, eye pain, blurred vision, loss of vision, watery eyes, halos
- Treatment might include eye drops, medication, surgery, or laser treatments
When to Call a Doctor
You should see an eye doctor every year or if you have any changes in vision. But if you have these symptoms, it could be an emergency.
- Blurred vision
- Black spots or “holes” in your vision
- Flashes of light
How to Manage Vision Loss or Blindness
Early Vision Loss
Magnifiers can help with early vision loss by enlarging the print in books and magazines. Hands-free magnifiers are especially helpful for reading, viewing the computer screen, and other activities. You can even get a magnifying mirror to help you see when applying makeup or while shaving.
Objects with large print are also helpful. Many libraries offer books with large text to make reading easier for people with vision problems. Other solutions include clocks with big, bold numbers and larger remotes with more visible buttons. Many pharmacies can print pill bottle labels with larger instructions.
A higher contrast between two things can also make it easier for people with vision loss. There are keyboards with contrasting colors between the large keys and the letters that making typing less difficult. The same principle can be used while eating. Eat lighter colored foods on darker plates and darker colored foods on lighter plates. This makes the food more visible. Some high contrast plates have edges to keep food from falling off your plate.
These visual aids can help you manage early vision loss. If your eye problems worsen, different tools might be needed.
Further Vision Loss or Blindness
Talking Devices
As your vision worsens, talking devices can help you with daily tasks. Both talking watches and talking alarm clocks can let you know what time it is. There are several products that are available in talking versions including tape measures, thermometers, scales, calculators, audiobooks, and microwaves. Use a talking blood sugar meter that can repeat the results and recall previous tests. A talking medication organizer can also be useful for reminding you when it’s time to take your pills.
Devices with Braille
If you know braille or plan to learn, devices with braille can also help you stay independent. It can be helpful to have a phone with braille to call people or a pill organizer with braille so you can tell which pills to take every day. You could use a braille labeller to label canned foods or playing cards with braille if you enjoy card games.
Using Pens to Inject Insulin
When it comes to injecting insulin, switching from vials to pens can make your experience easier. Insulin pens are pre-measured, so you know you’re getting the appropriate dose. This is often less challenging than measuring it out when using a vial.
Adaptive Cooking Devices
Adaptations can also help you cook and eat with vision loss. A cutting board with an attached knife is a safer alternative for cutting and chopping food. When eating, a plate with an edge can make it easier to scoop food without spilling. Many people picture the plate as a clock face to organize their food and remember where everything is on their plate. Other dining tips include holding a finger at the rim of the glass so you know when to stop pouring cold liquids, using salt and pepper shakers that are different shapes to identify them with ease, and making sure your knife rocks back and forth (this will mean the blade is facing down) before cutting.
Using a Mobility Cane
One last suggestion is a mobility cane. This probing cane can warn you about obstacles, stairs, and curbs that are ahead of you. They are typically lightweight and come in both folding and non-folding options.
Coping with vision loss or blindness can be challenging, but the right tools can make it less difficult to adapt.
Foot Problems
Why does diabetes cause foot problems?
Two main complications of diabetes can cause foot problems: diabetic neuropathy and peripheral artery disease.
Diabetic Neuropathy
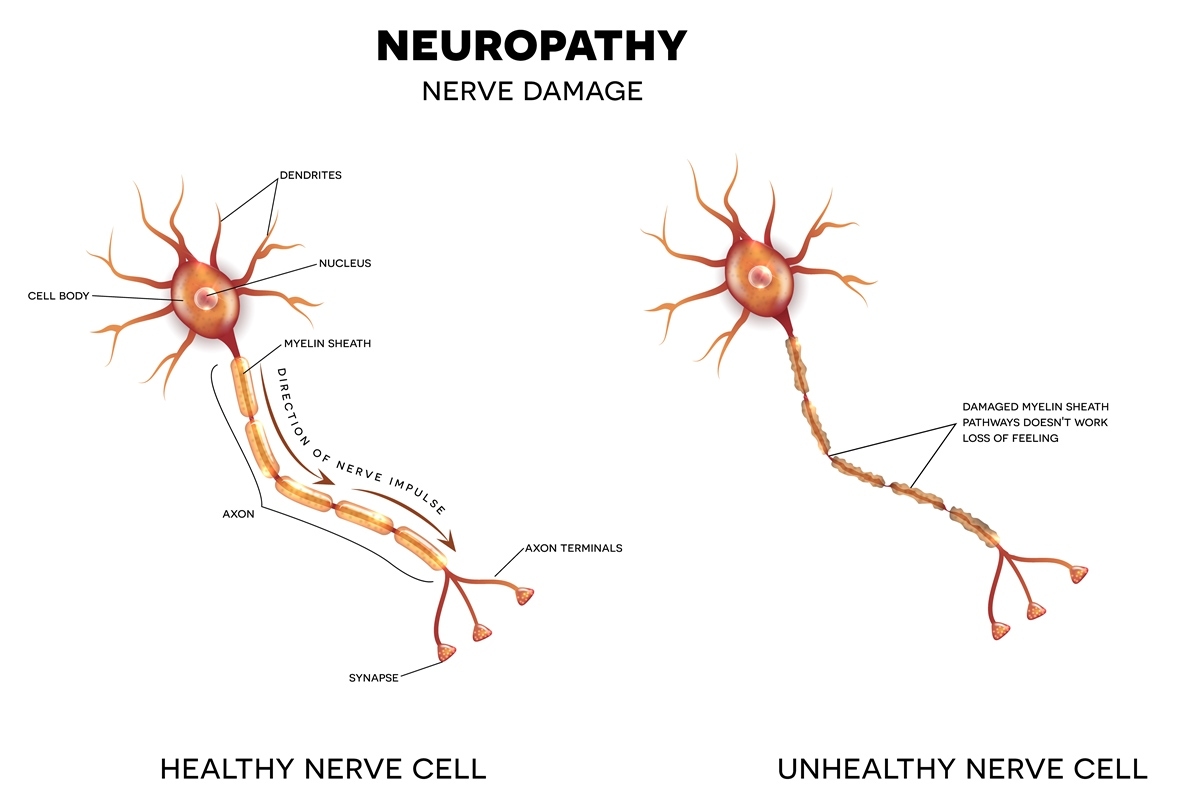
Diabetic neuropathy (nerve damage) is most common in the feet and legs. It occurs when the nerves in your body are damaged and can no longer feel sensations, like pain or touch. The damage means you won’t feel a cut or sore on your foot, which could become seriously infected and, if not treated, lead to amputation. This condition affects 60-70% of people with diabetes.
Peripheral Artery Disease
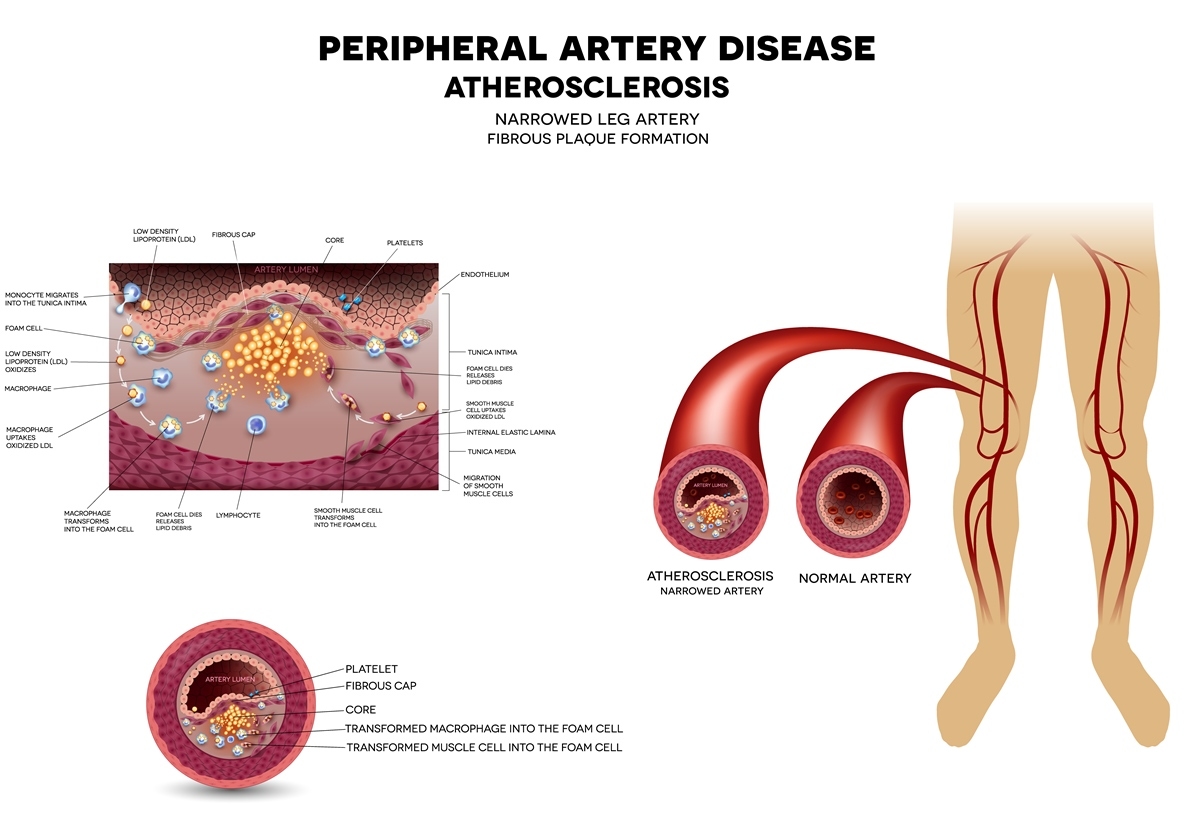
In the second condition, peripheral artery disease (PAD), your arteries have narrowed and are affecting your circulation. If you do get a cut while having PAD, it will take longer to heal, and an infection can turn into an ulcer or gangrene.
Together, the diseases put you at risk for foot problems. In the United States, diabetes is the leading cause of foot amputations. Thankfully, proper foot care and greater awareness has decreased limb amputations by 50% over the past twenty years in the U.S.
When to Call a Doctor
If you have any of these symptoms or warning signs, call a medical professional immediately.
- Burning, tingling, or pain in your feet
- Loss of sensation (heat, cold, or touch)
- The beginning of red spots, blisters, sores, ulcers, or ingrown toenails
Prevention
How to Protect Your Feet
Diabetic Socks
It’s important to protect your feet to prevent sores and blisters from developing. Luckily, there are a few ways to do this. One option is diabetic socks that protect your foot from the pressure that causes blisters and ulcerations. Some have gel for extra cushioning and support. It is also important to have proper-fitting shoes. They shouldn’t rub on your skin or pinch your toes.
Orthotic Insoles
Orthotic insoles can be added to your shoes for additional protection. One study found that using orthotics dropped the reulceration rate from 79% down to 15%. The amputation rate also decreased from 54% to 6%. Many orthotics fit into your existing shoes, and you can choose between high-end orthotics and lower priced alternatives. Consult your doctor for which orthotics are the best option for you. Additionally, you should always have some protective covering over your feet to prevent injury. Socks and shoes are the best option, even indoors, but slippers are another comfy option. Thermal slippers combine this protection with heat for improved circulation.
Protecting your feet can stop sores and cuts before they appear. Even with socks and orthotics, it’s important to look after your feet daily.
How to Care for Your Feet
Inspection and Washing
Carefully inspect your feet every day for any potential problems. If you can’t see part of your foot, use a mirror for inspection. Wash your feet daily to prevent bacteria from causing infection. If washing your feet is a struggle, a long handled foot sponge can help you reach. Moisture can lead to infections, so dry the area carefully, and make sure you check between your toes during your daily inspections.
Nail Care
If your nails need to be cut, after your shower or bath is a great time to do it. Cut straight across using a toenail clipper and then carefully file them so the nail is smooth. Long handled nail clippers make this task easier if you can’t bend or have limited mobility. Afterward, you can apply lotion to the tops and bottoms of your feet to keep them from becoming dry and cracked. Use a lotion applicator if it’s hard to reach, and avoid the area between your toes.
Careful care and monitoring will let you know if there are any problems with your feet. Contact your doctor if you have any symptoms so you can begin treatment before the cut or sore worsens.
Coping & Care After an Amputation
Mobility Aids
After a lower limb amputation, you might need crutches, a walker or a wheelchair to move around. Eventually, you might transition to using a prosthetic after the wound heals and you no longer need a mobility aid. Additional aids like a transfer bath bench can make other tasks like showering simpler.
Dressing Aids
Getting dressed might be more difficult after your amputation, but there are tools that can help. A dressing stick can help you pull shirts and pants into place when you get dressed or undressed. Putting on pants? The Sammons Preston EZ Dresser makes it easier by opening up the waistband so you can more easily get your legs inside. To reach clothing or other objects that fall on the ground, use a reacher, a long stick with a strong jaw on the end for grabbing items.
Transfer Aids
Another struggle can be getting in and out of bed. Transfer boards simplify moving from your wheelchair to your bed and back. Some have handles that let you stabilize yourself while moving. Once you’re in bed, a bed pull helps you move around and reposition yourself.
The best treatment for chronic diabetes complications is to control your blood glucose and talk to your doctor if you have any symptoms. Early treatment can prevent vision loss or foot damage from worsening. If complications arise, there are a variety of assistive devices that can help you maintain your independence.
References
Gonzalez Fernandez, M. L., Morales Lozano, R., Gonzalez-Quijano Diaz, M.I., Gonzalez Jurado, M. A., Martinez Hernandez, D., and Beneit Montesinos, J.V. (2013). How Effective Is Orthotic Treatment in Patients with Recurrent Diabetic Foot Ulcers?. Journal of the American Podiatric Medical Association. Retrieved from http://bit.ly/2EIhnTl
“How to Protect Diabetic Feet”. (2017, March). Retrieved from http://bit.ly/2ofY4GA
MedlinePlus. (2017, December). Diabetic Eye Problems. Retrieved from http://bit.ly/2faCo96 National Eye Institute. (2015, September). Facts About Diabetic Eye Disease. Retrieved from http://bit.ly/1GLSaz7
Medical Disclaimer: The information provided on this site, including text, graphics, images and other material, are for informational purposes only and are not intended to substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other healthcare professional with any questions or concerns you may have regarding your condition.








 France
France Australia
Australia






