Both pelvic floor physical therapy and dry needling have reached fever pitch in the media as well as in the blogosphere. Both are important in that they are changing the way that we treat and manage a variety of conditions that we have yet to have good answers for.
Dry needling can be utilized to help change the physiology of the tissues that the needles are applied to by increasing blood flow, increasing or decreasing muscle tension, and affecting the nervous system at the level of both the spinal cord and the brain.
Pelvic floor therapy is a broad term that defines a group of treatments used to address a variety of diagnoses. These diagnoses include bowel, bladder, and sexual dysfunction.
Because of the effect on both muscle pain and the nervous system as a whole, dry needling can be utilized as an effective tool to address dysfunction of the pelvic floor. In this article we will talk specifically about pelvic pain.
Pelvic pain is classified under a variety of diagnoses, including things like pelvic and perineal pain (R10.2) and dyspareunia (N94.1), or proctalgia fugax (K59.4), or pudendal neuralgia (G58.8).
These diagnoses are complex and often difficult to treat, leaving people feeling at the end of their ropes as they strive to manage the symptoms that they are afflicted with on a daily basis. Dry needling can effectively treat many of the things that are associated with those diagnoses.
This may be most easily illustrated through a case study. Anne is a 25-year-old female who arrived for physical therapy with a diagnosis of dyspareunia. She described systems of pain with initial insertion as well as pain that limits her ability to attend work and participate in her daily activities during her period. These symptoms have been present since she started menstruating at the age of 16 and she describes her inability to have intercourse as very distressing to both her and her partner.
On a more regular basis, she determines what clothing she chooses to wear based upon discomfort with wearing pants that are too tight around her waist, or underwear that is not cotton. She has also been unable to participate in recreational exercise, like running, that she used to help with maintaining her mental health.
Anne arrived for PT and during the initial evaluation we discovered that she had increased myofascial tension throughout her abdomen and upper thighs. She also had muscle tension throughout her abdominal muscles, and she described radicular symptoms in the S2 nerve route pattern, so down the back of her legs, often clear down into the posterior aspect of her heel.
At this time, she was utilizing pain medications to address her symptoms but found that they were doing nothing more than diminishing her pain and not increasing her function.
In physical therapy we started with myofascial release, exercises, and stretches, diaphragmatic breathing, and discussion of lifestyle changes, including things like getting appropriate sleep and taking care of her body, stress management, etc.
She is implementing each of these techniques on a regular basis as prescribed within her physical therapy plan of care and as a result her symptoms diminished from an every-day occurrence to only at the times of the month like when she was ovulating the two days prior to her period, and with vaginal insertion.
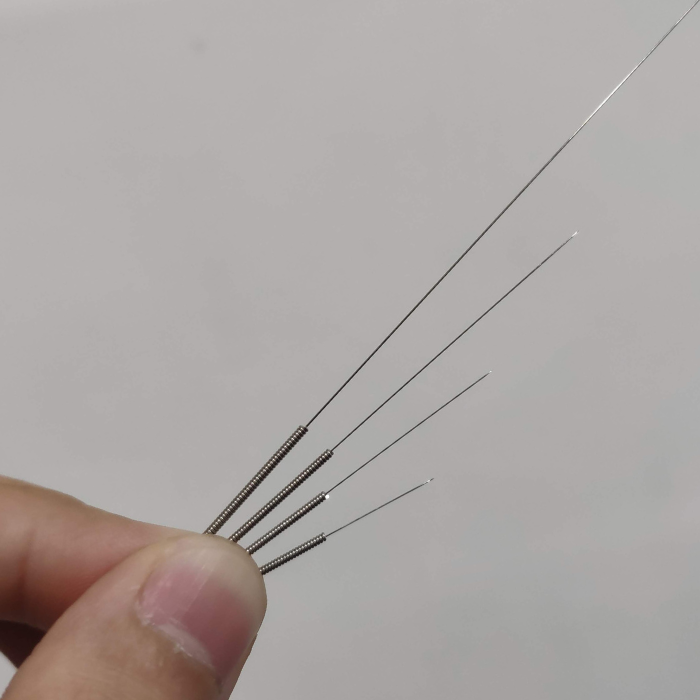
We discussed her willingness to trial dry needling. The purpose of dry needling at this point was to decrease muscle tension in and throughout the pelvic region, including her levator ani, coccygeus, as well as deep hip rotators. All these muscles can cause tension in and throughout the area surrounding the Sacral Nerve root two, which could be the cause of some of her radicular symptoms, as well as the cause of pain with initial vaginal insertion. Additionally, we utilized needles perineally to decrease tension in the superficial perineal transverse muscle, bulbocavernosus and ischiocavernosus.
While she described the needle insertion as acutely painful after about 48 hours the stiffness and tension that she had been unable to address with generalized stretching and other techniques resolved.
After one session of dry needling, she reported an additional 25% improvement of her symptoms, and what we needed to do was wait for a full menstrual cycle to assess what the hormonal fluctuations would do to her symptoms.
That menstrual cycle was the first that she had that was not acutely painful with ovulation, and she was able to manage the initial pelvic pain and cramps with fewer doses of medication.
So, what should inform your decision to utilize dry needling for patients with pelvic floor dysfunction?
Primarily, it is important that both the practitioner as well as the patient feel comfortable and confident, and that the practitioner has adequate training in both safety and technique to complete the needling protocol.
Assuming that those things are met, I often utilize dry needling as an adjunct to a full plan of physical therapy care, which would include other hand-on techniques: exercise, both stretching as well as strengthening, and stress management. In the absence of those additional things dry needling will often become a temporary solution as opposed to part of a permanent fix.
Dry needling is not often my first line of care, mostly because it becomes something that is able to enhance the other things that are being done, and it allows the patient to feel a sense of self-efficacy in managing their symptoms. Dry needling for pelvic floor dysfunction often takes several treatments to provide long-lasting relief and may require longstanding occasional treatment as well.
However, a patient's response to an initial needling session is something that should be considered. First, if a patient has a negative response, then needling should not be utilized. Needles are not magic, but they are a powerful tool.
If a patient has a good response to needles but they are looking for more, changing the dosage of the needling by increasing the number of needles, increasing the length of the lesion, or increasing the duration the needles are in situ can be helpful.
Additionally, in the posterior chain and lumbar spine, needle manipulation can sometimes help increase the dosage. In the perineum and the pelvic floor, needle manipulation is not advisable as it is poorly tolerated.
While dry needling in pelvic pain is something that is not utilized by all practitioners, it certainly is something that can provide relief in the absence of full relief being found with other treatments. It is absolutely a worthwhile tool to be added to a practitioner's toolbox.
Find pelvic health solutions and dry needling products on our website!








 France
France Australia
Australia