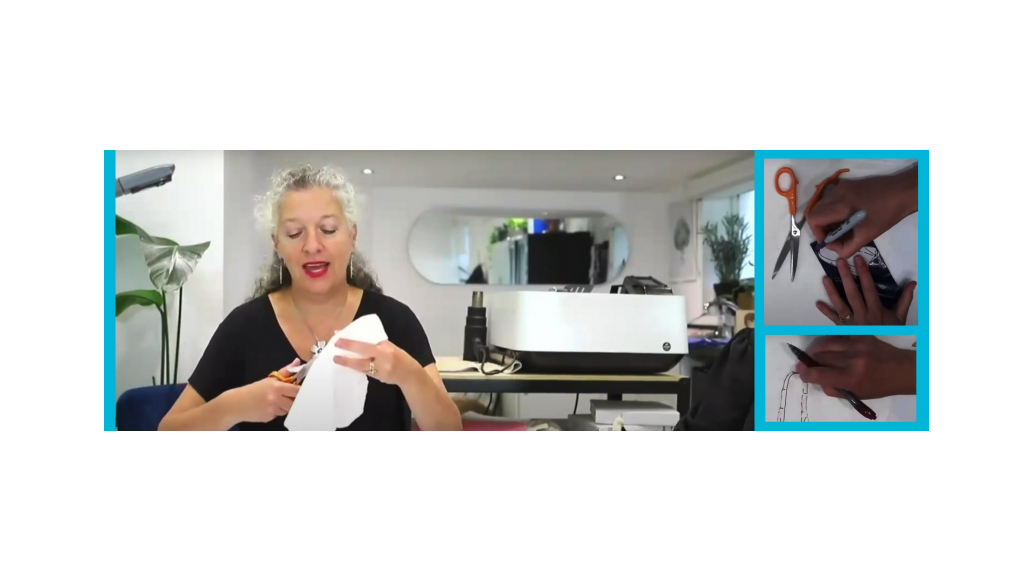
Join our webinar featuring Nicola Goldsmith, MSc, SROT. Most thermoplastic splints are made on the volar surface of the fingers, hand, wrist and forearm. In this webinar, we will explore some of the clinical and biological reasons for splinting on the dorsal surface. This will include rationale such as leaving the sensate area of a finger free, preventing pressure on wounds, and good lever arms for contracture. Conditions which will be discussed include mallet injury, post Dupuytren’s surgery and PIPJ contractures.
View the Recording of the Webinar
Q&A Between the Audience and Expert
1. Can you remind us of the different foams utilized in the video?
Temper Foam comes in pink and blue in a pack of two in a typical splint material size. I use the pink foam for padding, as it’s very soft and not very dense, but it will help distribute the pressure. Blue, I use more when I’m trying to add a bit of pressure and spread it across the anatomical area, which is double the density of the pink foam. I also use Hapla Fleecy Web, which comes in a roll or in pre-determined pieces. I also use called Hapla Fleecy Foam, which has an adhesive back, but still foam on the inside.
2. Can you tell us what thicknesses of Polyflex there are and who supplies it?
Polyflex is a Performance Health material, as are all the splinting material shown here. Polyflex comes in three thicknesses, 1.6mm, 2.4mm, and 3.2mm.
3. How does a patient safely remove and reapply at home?
In relation to the mallet finger splint, I teach the patient to press the tip of the finger into a tabletop. Then, use short blade scissors to carefully snip away along the facing side of the splint. The finger remains on the table the whole time. I have prepared a second splint (which they swap back and forth) and five pieces of zinc oxide tape. I also have a baby wipe available so they can clean their fingers. They gently lift the splint from the back of the finger, clean the finger, and place the new one on top. The tape is ready and can then be applied. I get them to practice this procedure on day one when it doesn't matter if the tip of the finger slips. I also record the process for them.
You will also find a video to help guide them on the amazing App "Hand Therapy" developed by the Chelsea and Westminster team. This app is free to use.
4. Would this dorsal splint work if a person has chronic mallet injury of about 6 years and now is developing mild swan neck deformity? For how many weeks does he need to use the splint to get complete recovery including DIP joint extension??
If the origin of the swan neck deformity was 6 years ago, and the tendon remains ineffective, no amount of splinting would help restore normal anatomy. It is far too late. I would maintain passive extension of the DIP and use a swan neck splint to manage the PIPJ.
5. Will you be able to send a pattern for this splint? It is more complicated, and I am having trouble replicating it.
Sorry - it is not possible to send patterns. Each splint should be made from the first principles of pattern making and individualized for each patient. Please look up some of my previous webinars (linked at the bottom of this article) on splinting to see more pattern making.
6. Could I ask what the name of the article is please? Would love to read.
7. I recently had a patient who had a simple dorsal mallet splint-fitted in France. They had superglued it to his nail and with a proximal turn of tape to secure it. Have you ever come across this? We had to soak it in acetone to remove it.
Oh goodness no. I have seen worse, with a Kleinert loop attached THROUGH the pulp of the finger.
8. Why do you prefer half-dorsal and half-volar based for Dupuytren's, is it for compliance/comfort or to give the soft tissue stretch?
It is not that I prefer it, it is an option. I think this style reduces the pressure on the healing wound, allows more airflow and less sweating, and it also gives a little lever.
9. In my hospital, we use a volar hand-based splint for all Dupuytren's post op patients. Do you recommend using the way you showed instead?
Each patient should be considered individually rather than doing the same technique all the time. I think this style reduces the pressure on the healing wound, allows more airflow and less sweating, and it also gives a little lever.
10. Do you ever use closed-cell foam for long term use to enable cleaning of the foam?
I prefer to change the foam. However, this is rare as I rarely use any inside a splint.
11. I love your dorsal serializing splint. Could you use this in reverse to increase PIP flexion? I have a patient with a severe comminuted fracture at base of MP and is so stiff - cannot flex at all. I would welcome your opinion!
With this situation, if the joint is very stiff, I would follow the advice on low load, prolonged stretch and use a volar splint, which was fashioned to be angled slightly more than the finger. Then use careful dorsal strapping. Slowly, slowly. No force required.
12. Can we see you make the thumb attachment on the last splint?
Here is the splint with the thumb piece added. It is measured as you can see. I have done it in black, so it shows well. Contour around the thumb and lightly tack to the main splint. Then, once the shape is holding, lift the phalange which is lightly tacked on and use a heat gun carefully and quickly on both sides to then press them into each other for a permanent bond.


Products Featured in the Webinar
More resources on splinting, Rolyan, and more:
Why Clinicians Choose Rolyan for Hand Therapy | Performance Health
Introducing the Rolyan Smart Splint Bath: Key Benefits | Performance Health
How to Choose the Best Splinting Material for Your Patient | Performance Health
Medical Disclaimer: The information provided on the site, including text, graphics, images, and other materials are for informational purposes only and are not intended to substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other healthcare professional with any questions or concerns you may have regarding your condition.








 France
France Australia
Australia