Key Takeaways
- Early Mobilization is Crucial but Faces Barriers: ICU patients, particularly those on ventilators, experience mobility challenges due to isolation, delirium, staffing shortages, and equipment limitations, leading to prolonged hospital stays, increased costs, and severe complications.
- Innovative Safe Patient Handling (SPH) Interventions Are Needed: Evidence-based mobility programs, such as the ABCDEF Bundling framework, help integrate rehabilitation into patient care. However, logistical barriers, including resource constraints and workflow integration challenges, hinder widespread implementation.
- Portable Parallel Bars Provide a Transformative Solution: This mobile, foldable device enables bedside therapy, allowing patients to stand, balance, and regain strength earlier in recovery. It reduces the need for gym transfers, enhances safety, and restores patient dignity while alleviating clinician workload.
- Real-World Impact and Call to Action: Preliminary feasibility surveys show high clinician satisfaction, improved patient mobility, and seamless integration into existing protocols. Expanding the use of these bars across ICUs, acute care, skilled nursing, and home settings can revolutionize rehabilitation and improve long-term patient outcomes.
Addressing the Critical Need for Early Mobilization
Early mobilization is fundamental to improving patient outcomes, reducing length of stay, and preventing hospital-induced complications.1,2 However, patients, particularly those on ventilators or continuous monitoring, face significant mobility barriers. Isolation, delirium, patient compliance challenges, and staffing shortages contribute to deconditioning, prolonged hospitalizations, increased costs, and severe health complications, including pressure injuries, respiratory decline, and cognitive impairment.
The COVID-19 pandemic exacerbated these challenges, underscoring the urgent need for innovative early mobility solutions. Annually, over 5 million ICU patients are admitted, with older adults and those with cardiac, respiratory, or neurological conditions being most affected.3 Ventilated patients, comprising 20–40% of ICU admissions, often lack access to critical standing and balance exercises essential for recovery.
Falls alone cost the U.S. healthcare system $50 billion annually, reinforcing the need for Safe Patient Handling and Mobility (SPHM) solutions to enhance recovery and reduce costs.4 Unfortunately, early mobilization efforts face multiple barriers, including patient instability, resource limitations, staff attitudes, and the need for specialized equipment that facilitates safe and effective therapy.5
Innovative SPHM Interventions in ICU and Acute Care
Effective rehabilitation requires structured, evidence-based interventions tailored to patient needs. Programs such as the ABCDEF Bundling6 framework and the Veterans Administration Mobility and Screening Tool7 systematically integrate mobility protocols into clinical workflows, reducing hospital-acquired deconditioning and improving recovery outcomes. Interdisciplinary training, hands-on workshops, and assistive technology utilization are critical to ensuring proficiency in mobility protocols. However, logistical barriers—such as limited resources and the challenge of integrating SPHM equipment into daily workflows—often hinder widespread implementation.
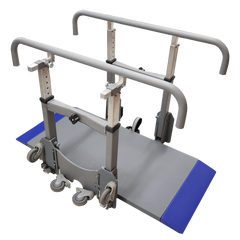
A Novel Solution: Portable Parallel Bars
To address these challenges, Portable Parallel Bars were developed in collaboration with physical and occupational therapy experts from the Veterans Health Administration. Peter DiSalvo, a physical therapist at the Richmond VA, collaborated to help invent and design these portable parallel bars.
This mobile, foldable, and wheeled device enables bedside therapy, removing many traditional mobility barriers.
By facilitating standing, balancing, and strength-building exercises at the bedside, the Portable Parallel Bars eliminate the need for labor-intensive and timely transfers to therapy gyms. Early clinical feedback highlights ease of use and increased patient and clinician confidence, leading to earlier and more effective rehabilitation.
"We’ve gotten good use of this equipment with great results. Easily transported to the room, easily set up and has been successful with patients who are max assist."
~Michelle Russo, PT Director of Rehab Medicine, Thomas Jefferson Hospital
Particularly beneficial for trauma, neurological, bariatric, SCI, and pediatric patients, the device supports a broad spectrum of mobility-impaired populations. Additionally, it restores patient dignity by enabling activities like bedside commode use, potentially reducing complications such as urinary tract infections (UTIs).
For clinicians, the device mitigates workforce challenges. Manual patient handling is responsible for over 55% of workers’ compensation claims, costing hospitals $4 billion annually, with lower back injuries being the most common8. The Portable Parallel Bars reduce physical strain by empowering patients to independently bear weight, holding onto the equipment and not the caregiver. Staff report workflow efficiencies, claiming “I can do more with less”, making this mobile tool a practical, scalable solution for numerous settings, including ICU and acute care.
Clinical Feasibility and Real-World Impact
Preliminary feasibility surveys demonstrate strong support for the Portable Parallel Bars, with clinicians rating it an average of 5.5 out of 6 on a Likert scale for safety, usability, and recovery impact. Key benefits include:
- Enhanced Safety and Confidence: Clinicians report secure handling, and patients regain mobility with greater confidence.
- Improved Accessibility: Bedside therapy is more immediate and effective.
- Seamless Integration: The device fits naturally into existing SPHM protocols.
- Positive Recovery Outcomes: Early adopters observe improvements in mobility, even in complex cases.
- High Clinician Endorsement: Strong recommendations from healthcare providers highlight its transformative potential.
Real-world applications span diverse patient populations and care settings. Integrated into ICUs, acute care, skilled nursing, and outpatient rehabilitation, the Portable Parallel Bars are reshaping mobility therapy. By allowing patients to stand, balance, and build strength at their bedside, the bars reduce both physical and emotional strain associated with traditional therapy routines. Their potential for home use further extends benefits to aging adults and individuals with chronic mobility impairments, enabling sustained independence and quality of life improvements.
Call to Action: Advancing Early Mobility Initiatives
The Portable Parallel Bars represent more than just an assistive tool—they are a catalyst for improved patient outcomes, clinician safety, and healthcare efficiency. Healthcare leaders, policymakers, and providers must prioritize the adoption of early mobility solutions and invest in technologies that bridge gaps in patient care. By integrating these advancements into SPHM protocols and expanding their use in home health, we can drive meaningful improvements in patient recovery and quality of life. Now is the time to take confident strides toward improving mobility access and eliminating challenges that impede recovery, dignity, or independence.
Top Product in this Article
More Recommended Products
References
- Hartley PJ, Keevil VL, Alushi L, et al. Earlier Physical Therapy Input Is Associated with a Reduced Length of Hospital Stay and Reduced Care Needs on Discharge in Frail Older Inpatients: An Observational Study. Journal of Geriatric Physical Therapy. 2019;42(2):E7-E14.
- Klein K, Mulkey M, Bena JF, Albert NM. Clinical and psychological effects of early mobilization in patients treated in a neurologic ICU: a comparative study. Crit Care Med. 2015 Apr;43(4):865-73. doi: 10.1097/CCM.0000000000000787. PMID: 25517476.
- Viglianti EM, Iwashyna TJ. Toward the Ideal Ratio of Patients to Intensivists: Finding a Reasonable Balance. JAMA Intern Med. 2017 Mar 1;177(3):396-398. doi: 10.1001/jamainternmed.2016.8476. PMID: 28118655; PMCID: PMC5856229.
- Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. 2018 Apr;66(4):693-698. doi: 10.1111/jgs.15304. Epub 2018 Mar 7. PMID: 29512120; PMCID: PMC6089380.
- Dubb, R., Nydahl, P., Hermes, C., Schwabbauer, N., Toonstra, A., Parker, A. M., Kaltwasser, A., & Needham, D. M. (2016). Barriers and strategies for early mobilization of patients in intensive care units. Annals of the American Thoracic Society, 13(5), 724–730. https://doi.org/10.1513/AnnalsATS.201509-586CME
- Marra A, Ely EW, Pandharipande PP, Patel MB. The ABCDEF Bundle in Critical Care. Crit Care Clin. 2017 Apr;33(2):225-243. doi: 10.1016/j.ccc.2016.12.005. PMID: 28284292; PMCID: PMC5351776.
- Melillo, C., Rugs, D., Toyinbo, P. et al. Reliability and validity of the Veterans Administration Mobility Screening and Solutions Tool. BMC Health Serv Res 22, 1323 (2022). https://doi.org/10.1186/s12913-022-08745-1
- Darragh AR, Campo M, King P. Work-related activities associated with injury in occupational and physical therapists. Work. 2012;42(3):373-84. doi: 10.3233/WOR-2012-1430. PMID: 22523031; PMCID: PMC3839086.
Medical Disclaimer: The information provided on this site, including text, graphics, images, and other material are for informational purposes only and are not intended to substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other healthcare professional with any questions or concerns you may have regarding your condition.








 France
France Australia
Australia