Key Takeaways
- Supply chain costs represent 40-45% of a healthcare system’s operating expenses, but proper supply chain management can reduce the cost by 5-15%1
- Healthcare supply chain management consists of analyzing your medical supplies activities to provide the best possible patient care while considering the value of all costs
- Standardization is one way to help manage your supply chain costs
- Standardization is a process often overseen by a value analysis team to choose healthcare products and services considering evidence-based results, to ensure quality patient care and fiscal responsibility
- There are many ways you can reduce variation while selecting best-in-class products, driving optimal clinical practices, reducing patient risk, reducing costs, and more!
Top Products in This Article
- Statistics: The Rising Costs of Healthcare & Supply Chain Savings
- What is the supply chain and supply chain management?
- What is standardization?
- Why is standardization good for your hospital or clinic?
- Why is standardization sometimes disliked by clinicians and physicians?
- What do you need to consider when beginning standardization?
- What considerations are often missed when standardizing?
- Potential Standardization Challenges and How to Overcome Them
- Other Ways to Reduce Costs
- How Performance Health Can Help You Standardize Your Products
Statistics: The Rising Costs of Healthcare & Supply Chain Savings
Share this infographic to spread awareness about the facts and benefits of standardization!

- Gartner Research states that supply chain costs are continuing to escalate and represent 40-45% of hospital/healthcare system operating expenses1
- Unnecessary hospital spending on supply chain products and related operations and procedures has reached about $25.7 billion a year, according to an annual analysis by Navigant2
- Gartner estimates that healthcare organizations can reduce those costs by 5-15% with better planning and control of their supply chain management1
- According to an analysis by Navigant, for individual hospitals, the average total supply expense reduction dollar savings opportunity jumped to $12.1 million (as of 2019). This amount is equivalent to the average annual salaries of 165 registered nurses or 50 primary care physicians, or the average cost of 3,100 knee implants.2
- As one example of possible supply chain savings, Seattle Children’s Hospital realized savings of 20% per case in supply costs after implementing standardized preference cards for laparoscopic appendectomy.3
- A larger product conversion project at Intermountain Healthcare found that 24,000 items in their 100,000–line-item master were unique, meaning they were being used by only one facility or, in some cases, a single clinician. They developed a “Justify and Standardize” which along with other initiatives, helped Intermountain reduce purchase order lines and invoice lines, right-size its inventory, and lower costs based on higher utilization. Intermountain realized $1.5 million dollars in savings, thanks in large part to its standardization initiatives.4
What is the supply chain and supply chain management?

Supply Chain: Investopedia defines it as “A supply chain involves a series of steps involved to get a product or service to the customer. The steps include moving and transforming raw materials into finished products, transporting those products, and distributing them to the end-user. The entities involved in the supply chain include producers, vendors, warehouses, transportation companies, distribution centers, and retailers.” 5
Supply Chain Management: NC State University defines it as “Supply chain management (SCM) is the active management of supply chain activities to maximize customer value and achieve a sustainable competitive advantage.” 6
Healthcare Supply Chain Management: PODS for Business defines it as “the process of regularly optimizing medical supply activities to provide patients the best possible care while considering the value of all costs involved.” 6
What is standardization?
Standardization is often thought of as a misunderstood, negative term, a “cookie-cutter approach.” But the real goal is to improve the patient experience, increase patient safety, and minimize the risk of errors. It’s one way to help manage your supply chain.
In healthcare, standardization is “the process by which healthcare products and services are chosen by a committee of key stakeholders, considering evidence-based results, to ensure quality patient care while adhering to fiscal responsibility.” 7
There are four main types of standardization:8
1. Product Selection: Analyzing the supplies used in different procedures to choose those that offer the best price-quality value
2. System-Wide Standardization: As community-based healthcare delivery grows, healthcare systems must set up systems to manage supplies outside traditional acute locations
3. Standard Clinical Practices: To closely define how procedures are clinically performed, in an attempt to produce consistent patient outcomes
4. SKU Reduction: To reduce unused medical supply waste (redundant, unused, and expired supplies) by reducing the SKU list to only the most critical SKUs to help reduce carrying costs
Why is standardization good for your hospital or clinic?
There are many benefits to standardization within an individual facility and across a system including:
- Selecting best-in-class products
- Driving optimal clinical practices
- Reducing waste
- Increasing buying power
- Improving the quality and consistency of care
- Reducing patient waste
- Increasing efficiency
- Reducing costs
Why is standardization sometimes disliked by clinicians and physicians?

Different healthcare providers often have different thoughts about standardization.
Many physicians and clinicians see standardization as a means of control and do not embrace it without evidence of standardization benefiting patient outcomes. Some feel it is a one-size-fits-all approach that doesn’t take into consideration the idea that each patient should be treated as an individual. However, personalization can mean making each patient feel acknowledged as an individual rather than requiring individual product SKUs.
Others are concerned that standardization means agreeing to use a lower quality product or that it will upset their routine and confidence to use an unfamiliar product. But there are ways to overcome these challenges by partnering with clinicians when choosing products and reminding them that you both want to help patients afford care as well.
In contrast, many nurses think of standardization as a time-saver. The less time they need to spend searching for the proper equipment, the more time they can spend with their patients. They also see it as a focus on cost-savings, patient safety, and efficiency.
Patients typically believe standardization is for their benefit, but they care much more about the manner they are treated than the methods used to treat them.
What do you need to consider when beginning standardization?

If you’re part of the value analysis team there are many things to consider when beginning to rationalize SKUs to reduce variation without affecting patient outcome and satisfaction.
1. Consider all perspectives
When making decisions as part of the value analysis team, consider product procurement and distribution, mitigating the use of improper usage, reducing variability in clinical practices, providing the best patient outcome, and supporting the development of user competencies. You’ll want supply chain professionals, quality professionals, and clinical team members to all be part of the value analysis team to help discuss questions such as:8
- Does it support quality outcomes?
- Does it provide the best clinical value?
- Will it help staff be more efficient?
- What training is required?
- In the final analysis, will this product in comparison to others in the same class, be the best choice to help us deliver high quality, cost-efficient healthcare?
2. Choose a category to start with
This can be an overwhelming project. If you have multiple categories, choose a category to address first.
3. Reduce SKUs to create a leaner inventory
Identify low volume, high variability, low margin products, and look for opportunities to consolidate them with high volume, low variability, and high margin products. You should be sure to always offer at least two sources and selections for a product so there is always an alternative available.
4. Evaluate Physician Preference Items (PPI)
This is another source of duplication and excessive inventory. PPI products should be carefully evaluated to determine what items are “preference” driven vs. procedural requirement driven. Ask them to justify what unique SKUs need to be kept and standardize as much as possible. By partnering with physicians and clinicians you can work to offer education and training to gain acceptance and reduce inventory.
5. Reduce waste
Ensure the right products and the right quantities are used for different procedures. For example, ensure sterile products aren’t used for a non-sterile procedure and avoid opening a prepackaged kit to only use one item.
6. Standardize across systems
If you are a larger healthcare system, ensuring all units are buying the same products, when possible, helps leverage your purchasing power and reduce your overall supply chain costs.
7. Set policies around supply chain management
Set up policies and procedures covering everything from product selection and ordering to distribution and disposal.
8. Limit vendors
Choosing a specific group of vendors for all supplies helps reduce SKUs and create the opportunity for volume discounts.
9. Clinical standardization
Define and enforce clinical protocols to be used across the system.
10. Utilization
Another critical step is to ensure supplies are being used in the specified way, in the right amount, under appropriate circumstances. For example, if a dressing has a seven-day wear time according to the manufacturer, but the facility replaces dressings every three days, this is in important mismatch to identify. The value analysis team can then either change the policy so the product is used to its full potential, or select a different shorter-duration product (usually at a lower cost). Aligning products to protocols can reduce waste and costs.
What considerations are often missed when standardizing?
Some tips on potential standardization issues include:
- Manage your Lawson cycles
- If your facility uses Lawson numbers, you know that until all the products are depleted, a Lawson number can’t be removed. This means employees can see the number and keep ordering supplies, even if it’s targeted for elimination, creating a vicious cycle.
- Investigate like hospitals with unlike usage
- Data that shows a wide variety of product usage among hospitals with similar patient demographics and acuity levels suggest a possible standardization issue within your system.
- Don’t forget about kits
- Make sure if you standardize any products, the same products are included in your kits.
- Easireach II Reacher (26” or 32”)
- Plastic shoehorn
- Sock aid with built-up handles
- Contoured bath sponge
- Proper coding is key
- To extract proper data in order to make sound decisions, you need proper product coding. If masking and medical tapes are both coded in your system as “tape” it’s harder to extract insights.
- More versions = less mastery?
- Buying different brands of similar products can be wasteful not only in cost, but also in clinical competency. For example, “A New Jersey hospital found that of two similar products, product A was applied correctly to patients only 36% of the time, while product B was applied correctly 84% of the time.”8 Fewer variations in products makes it easier to master how to use them properly.
- Use one, not two
- Look for scenarios where your facility may be using two products when one can be used to get the same job done.
Potential Standardization Challenges and How to Overcome Them
Supply chain standardization can be difficult, get ready to tackle three of the most common challenges:
1. Managing Clinician Preference
Clinicians are the primary users and it’s crucial to involve them in the decision-making process. Their opinions can help find products that balance quality, clinical effectiveness, availability, and cost. Take a collaborative approach to reduce fears about lesser quality products and the need to become familiar with new products. You can provide comparative data on product effectiveness and patient outcomes and provide reassurance that quality patient care is everyone's top priority.
2. Realigning Your Product Master
Your product master may have accumulated duplicates, outdated supplies, and more over time. You’ll need to put in the work to update it and ensure you can identify each product, determine its correct usage, and cross-reference it against other similar products. This allows you to create a baseline for standardization discussions.
3. Changing Clinical Practice
For standardization to be most effective, you need to make changes in the clinical practices too. This may require the development of new protocols and policies related to how products are used in the clinical setting. As well as change management, training, and compliance monitoring to encourage and ensure the adoption of your new practices.
Other Ways to Reduce Costs
Aggregating your purchasing is another way to reduce supply chain costs.1
GPOs

Group purchasing organizations (GPOs) help healthcare providers realize cost savings by aggregating purchasing volume and using that leverage to negotiate discounts with manufacturers, distributors, and other vendors. GPOs combine the buying power of member hospitals to negotiate lower contracted prices than they could achieve on their own. “According to the Healthcare Supply Chain Association, approximately 72% of hospital purchases are now conducted through GPO contracts.”1 Because GPOs are closely aligned and often owned by their members, they share many of the same supply chain concerns and goals. They are another way to help reduce your costs.
Performance Health is contracted with most major GPOs.
Wholesalers and Distributors

Purchasing through wholesalers and distributors aggregates your purchase volume, improves efficiency, and reduces costs. You can receive your products from many vendors in a single order, shipment, and invoice. You can also work with wholesalers and distributors to develop replenishment models that meet your specific needs and circumstances, such as order size, delivery frequency, and distribution requirements.
Performance Health is the largest global manufacturer and distributor of products to the rehabilitation and sports medicine markets and delivers to over 1K points of care. Learn more about looking up invoices, tracking your orders, and more with these videos.
How Performance Health Can Help You Standardize Your Products



As the largest global manufacturer and distributor of rehabilitation and sports medicine products, Performance Health is the logical choice for rehabilitation and recovery providers. We offer a wide variety of best-in-class brands in #1 and #2 market positions, so you know you’re getting great value at a great cost. Plus, you can purchase from several different brands in a single order and invoice.
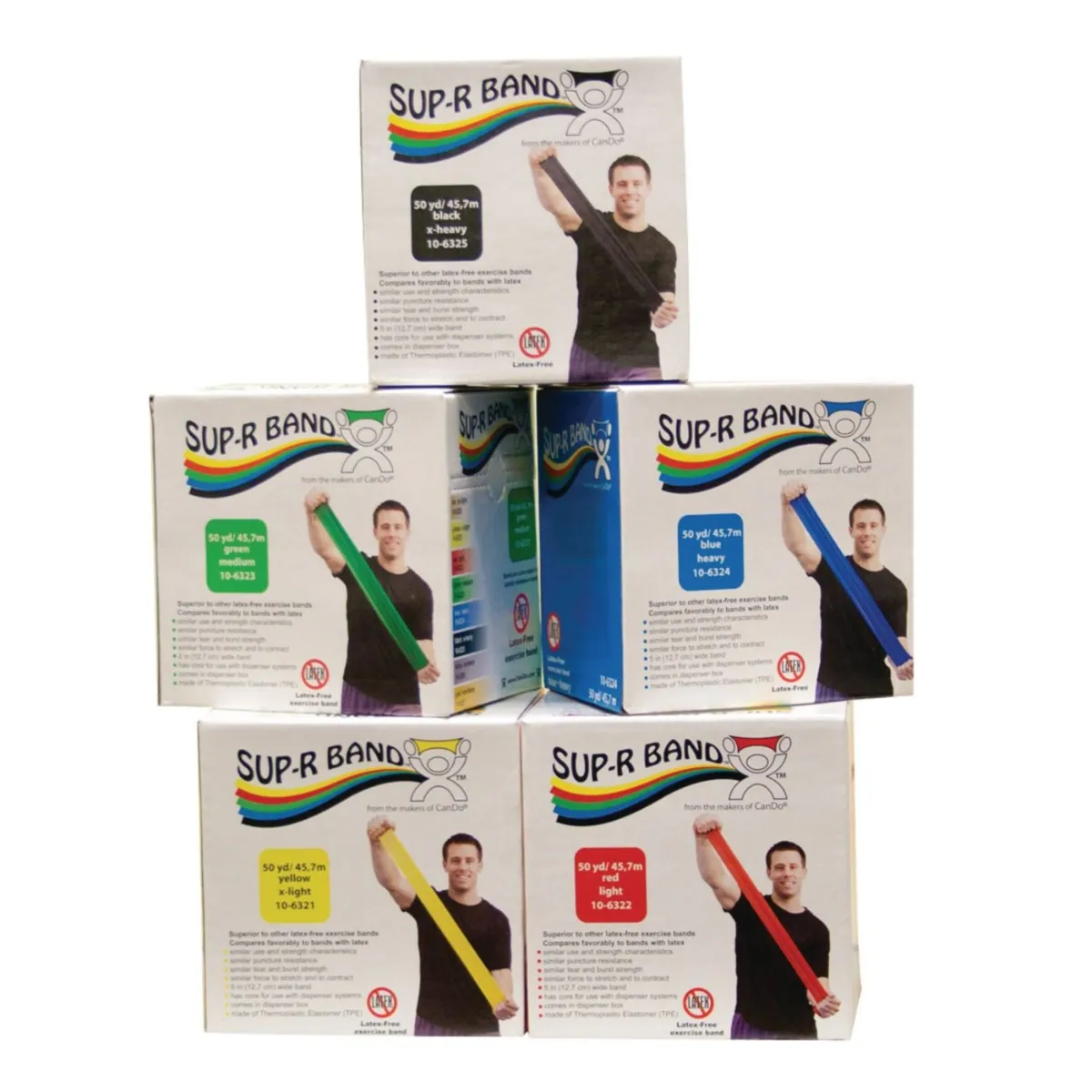
Our position as a manufacturer and distributor allows you to standardize products like resistance bands by choosing TheraBand Non-Latex Resistance Bands as your standard and an alternative like Rolyan Energizing Exercise Band Rolls or choosing Sammons Preston Reachers with Homecraft Handi-Reachers as an alternative. We also offer products made in the USA, like our thermoplastic splinting sheets.
Performance Health offers tools like Web Order Approval (WOA) that allows you to appoint a company admin to approve purchases and ensure orders are being placed only for the brands/products your value analysis team has chosen. Or use approved Supply Lists that make it easy for purchasers to see the products they should be buying.
If you’re interested in working to standardize your product assortment, your Performance Health sales representative would be happy to work with you!






References
1. Austin Allen. (March 2020). 5 Ways to Address Rising Healthcare Supply Chain Costs. Austin Allen. Retrieved from https://bit.ly/3msldCY
2. Lagasse, J. (November 2019). Unnecessary healthcare supply chain spending reaches almost $26 billion; savings opportunities remain. Healthcare Finance. Retrieved from https://bit.ly/3AkxTRg
3. Betcheva, L., Erhun F., and Jiang, H. (2020). Supply Chain Thinking in Healthcare: Lessons and Outlooks. Cambridge Judge Business School. Retrieved from https://bit.ly/3DvHneH
4. Straseske, B. & Bakemeyer, E. (January 2020). HBI’s Latest Report Focuses on Supply Chain Standardization. HBI. Retrieved from https://bit.ly/3BgeEcQ
5. Kenton, W. (August 2021). Supply Chain. Investopedia. Retrieved from https://bit.ly/3msah8u
6. Handfield, R. (February 2020). What is supply chain management (SCM)? NC State University. Retrieved from https://bit.ly/3iEtUJc
7. Stone, J. (January 2020). Defining Standardization and Personalized Care. MedicalGPS. Retrieved from https://bit.ly/2YoPdb4
8. 3M. (n.d.). Supply Standardization: The Clinical and Economic Benefits of Reducing Waste in the Supply Chain. 3M Healthcare. Retrieved from https://bit.ly/3BlirFR
Medical Disclaimer: The information provided on this site, including text, graphics, images and other material are for informational purposes only and are not intended to substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other healthcare professional with any questions or concerns you may have regarding your condition.








 France
France Australia
Australia



















