As cases of COVID in the U.S. rise to over 4.7 million, you may be wondering how to keep patients safe in your rehab clinic, long term care facility, or hospital.1 By planning ahead and following key measures including personal protective equipment (PPE), hand hygiene, disinfecting, social distancing, and other guidelines, you can help keep your patients protected during the pandemic.
|
Table of Contents
- 7 Preparation Steps to Protect Your Patients & Staff
- Personal Protection Equipment
- Hand Hygiene
- Social Distancing
- Cleaning and Disinfecting Exercise Equipment and Therapy Tools
- Disposable, Wipe Clean, Washable, and Antimicrobial Products
- How Will You Handle COVID-19 Exposures?
- COVID-19 Infection Prevention Summary
- Learn More About Infection Prevention
7 Preparation Steps to Protect Your Patients & Staff

1. Develop a Safe Workflow
Develop a written process for a safe workflow. Consider whether you will have patients enter through one door and exit through another. Walk through your clinic and consider what you can do to reduce contact between patients and staff.
2. Consider Your Waiting Room Policies
How will you protect patients in your waiting room? Will you have patients call to say they have arrived and then wait in their car until you call them to come in? Will you set a maximum occupancy for the number of people in the waiting room and implement social distancing? If you decide to use social distancing, will you remove additional chairs and space out the remaining? Or if you cannot move the chairs because they are bolted down, will you rope off some seats to allow for social distancing? Will patients fill out forms on a tablet instead of using paper and pens? If so, then the tablet will need to be disinfected after each use. These are just some of the things to consider when creating waiting room policies.
3. Screen Patients Prior to Visit
You can pre-screen patients and visitors online or by phone prior to their visit.
Ask questions such as:
- Have you been sick with any of these symptoms?3 Check all that apply.
|
|
- Have you come in contact with anyone with the above symptoms in the past 14 days?
- Are you in contact with anyone who has been confirmed to be COVID-19 positive?
- Have you traveled in the past 14 days to any regions affected by COVID-19? If so, where?
- Have you been tested for COVID-19? If yes, what was the result?
- Have you been diagnosed with COVID-19? If yes, when?
- Are you over the age of 65?
- Do you have:
- Heart disease
- Lung disease
- Kidney disease
- Diabetes
- Autoimmune disorders
You can have the patient fill out your questionnaire before their appointment, in person at the office, and again post-appointment to ask if they have developed symptoms or have been diagnosed with COVID-19 so you can handle potential exposures.
When your patients or visitors arrive at your facility, you can also conduct temperature checks.
Decide whether you would prefer to use disposable Tempa-DOT thermometers, disposable digital thermometers, standard digital thermometers with probe covers, like the Filac 3000 EZ Electronic Thermometer or Welch Allyn Sure Temp Plus 690 Thermometer, or a digital non-contact forehead thermometer.
Set a base temperature and have patients who test above that go home and reschedule their appointment for a later date. While the CDC recommends screening for a fever equal to or higher than 100.4°F they state that a lower temperature threshold (e.g., 100.0°F) may be used, especially in healthcare settings.4
4. Screen Staff and Set Up Sick Policies
You can use a similar questionnaire like the one above and temperature checks to screen your staff before work everyday.
Make sure your staff knows the procedures so they don’t work when sick. If you have an occupational health partner, you can partner with them to create staff procedures.
5. Post Visual Reminder Signs
Post professional pictorial signs on hand hygiene, wearing a mask, and social distancing in the waiting room and throughout your facility to remind your patients and staff of these important measures.
Consider posting signs limiting the number of people in an elevator at one time.
Decide if you will use social distancing floor decals to illustrate how far apart 6 feet is, the distance people should stand to social distance while in the elevator, waiting room, or any other common areas.
Communicate (by phone, email, etc.) what you are doing to keep everyone safe to ensure your patients and staff feel safe when coming to your clinic.
6. Require Masks and Encourage Hand Washing


Many clinics are requiring that everyone wear a mask. Patients and visitors are told to bring a cloth mask from home and wear it while in the building. Staff often wear a cloth mask in common areas and a disposable surgical mask when with patients. N95 respirator masks are typically not needed except during aerosol generating procedures.
Let your patients know that they will need to bring a mask when they schedule their appointment. Explain why it is so important for them to wear a mask to help prevent the spread of COVID-19. Remind your patients of the mask requirement again shortly before their appointment.
Be prepared to offer masks to patients who do not bring their own. Depending on your clinic and its budget, you may want to offer them for free or sell them. Many long term care facilities are providing cloth masks to their residents.
If your patient refuses to wear a mask, remind them it’s for their protection and everyone else's including yours. Ask questions to see why they are afraid or refusing to wear a mask. But ultimately state that it’s the clinic policy and refuse service if they won’t wear a mask.
Encourage frequent hand washing and sanitizing by your staff and patients. Have hand sanitizer readily available when patients enter your facility and in common areas such as in gyms or near elevators. Learn more about hand hygiene below.
7. Limit Visitors
Many facilities are limiting visitors. Some are only allowing visitors to critically ill patients while others are only allowing a parent to stay with a child patient. Others are allowing no visitors, this is more common in long term care facilities since there is such a high-risk population of elderly residents.
In ambulatory settings, many patients are cutting visits by choice. Some outpatient rehab centers are reducing the number of patient appointments to ensure social distancing in the gym.
Consider what is the right visitor policy for your facility.
Personal Protection Equipment

Ensure your facility has adequate personal protective equipment (PPE). This includes gowns, gloves, and surgical masks. Acute facilities may also use face shields. If your department performs many aerosolized procedures, you will also need N95 masks. There is currently a N95 shortage and for many procedures a surgical mask is adequate, depending on the procedure.
Your stock of PPE supplies should be checked daily to ensure you do not run out of needed supplies. Ensure you can source the PPE, consider how much you expect to go through in one day, and how much you project you will use in the future based on your patient population. The CDC has created a Personal Protective Equipment (PPE) Burn Rate Calculator to help facilities plan and optimize the use of PPE during the coronavirus of 2019.
Gloves and gowns should be discarded after use. Some facilities allow masks and face shields to be reused if the patient is not COVID-19 positive and not symptomatic. Consider whether you will allow your staff to reuse masks and create guidelines for if they can be reused and if so, how long they can be reused. For example, until they are wet, dirty, soiled as long as they are used with not-symptomatic, non-COVID positive patients.
- Masks
- Gloves
Hand Hygiene
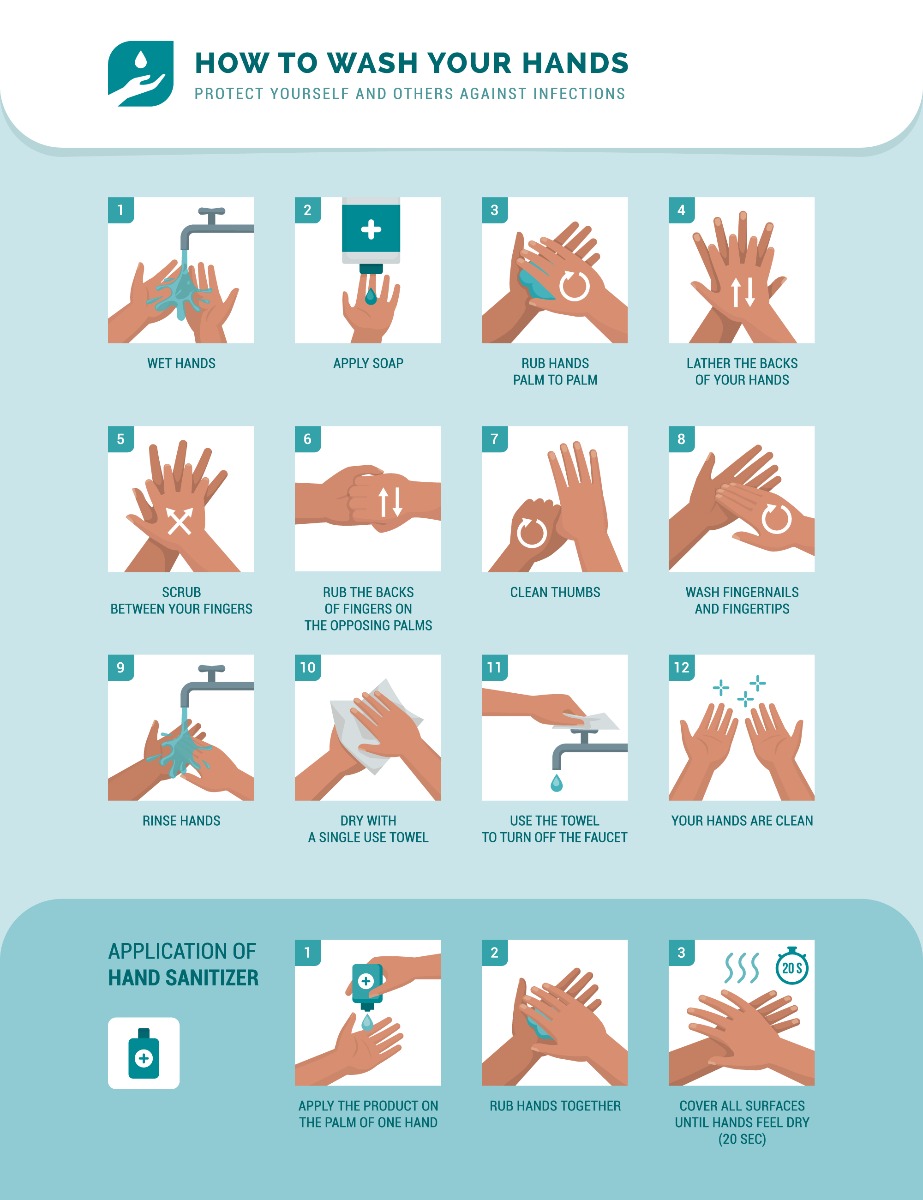
Frequent hand washing is a key measure to help reduce the spread of COVID-19. Encourage your staff to regularly wash their hands with soap and water for at least 20 seconds. Create guidelines for when your staff need to wash their hands, such as before and after contact with each patient during appointments, before and after entering each patient’s room, before applying and after removing gloves, etc.
If some of your staff has less frequent contact with patients, perhaps add a guideline with a time limit, such as washing their hands at least once an hour.
Ensure you have hand soap available for healthcare professionals and that the hand soap in patient and visitor bathrooms are filled. Post signs that remind patients and staff to wash their hands. You may want to include signs that show how to properly wash your hands as well. Remind everyone to avoid touching their eyes, nose, and mouth.
If soap and water are not available, use a hand sanitizer that is at least 60% alcohol, such as Purell Advanced Formula Hand Sanitizer, Germ War Hand Sanitizer, or 3M Avagard D Instant Hand Antiseptic. Make sure the hand sanitizer is easily accessible for patients and staff.
Decide if your staff can use just hand washing for manual therapy if the patient is not ill and there will be no contact with bodily fluids or if you will require them to use gloves. Consider the availability of your PPE supplies, whether your patients will expect glove use, and if it will make your staff members feel better. If you choose to have your staff wear gloves, ensure they know it is for one time use only and that the gloves can NOT be reused. You must decide based on your facility’s needs.
Social Distancing

Social distancing is another important part of reducing the spread of COVID-19. The coronavirus is thought to spread between people who are in close contact with each other, within about six feet. Post signs to remind staff and patients/residents to practice social distancing. The signs should be visual and remind everyone to stay the recommended 6 feet apart, even if they are wearing masks.
Make sure there is social distancing in the gyms and common areas, like waiting rooms. If necessary, reconfigure the room so people have space and aren’t sitting next to each other. This may include not allowing the use of some exercise equipment, depending on what’s in use, to avoid patients being too close together. If therapists will be using the room at the same time, encourage them to plan how they will use the space together while still implementing social distancing measures.
Social distancing floor decals can provide a visual reminder to stay six feet apart.
Cleaning and Disinfecting Exercise Equipment and Therapy Tools

You must have procedures in place for cleaning and disinfecting all shared equipment. This includes exam tables, gym mats, exercise equipment, and more. Between each use, equipment needs to be wiped down.
Be sure to build time to clean and disinfect equipment between patients into your schedule. Some rehab gyms can use less equipment, but it depends on your expertise and patient needs. If multiple people will use the gym at one time, make sure to follow social distancing guidelines.
Be sure your staff knows what disinfectant products can be used on each piece of equipment. In some cases, it may make more sense to make it the patient’s personal equipment. For example, a finger exerciser can be wiped down between patients but it makes more sense to label therapy putty containers or divide into individual personal Ziploc bags. TheraBand Resistance Bands can be cleaned in soap and water, but cutting individual lengths for specific patients can help save your staff time. Be sure to think about what makes the most sense for your patients and how you will store patient specific products to avoid cross contamination.
Coordinate with your environmental services team to ensure you are using the correct disinfectants for equipment, surfaces, and more. Traditional disinfectants can typically be used, check an EPA list of disinfectants for use against COVID-19. Other alcohol options may be approved for surface disinfection by your infection prevention and supply management team (for example, think of a distillery making hand sanitizer).
If you have a service that comes in to clean at night, evaluate your contracted cleaning service products and make sure they are using medical grade products. Also, ensure staff have clear direction on how to clean all shared therapy equipment.
When cleaning and disinfecting your space, these products might be helpful:
- Cavicide and Caviwipes
- Disinfecting Wipes 80ct, Case of 12
- PAWS Personal Antimicrobial Wipes
- Protex Ultra Disinfectant Solution
- Envirocide Disinfectant Cleaners
- Citrus II Germicidal Deodorizing Cleaners
- Wavicide Disinfecting Solution
- GymWipes Antibacterial Force Wipes
Disposable, Wipe Clean, Washable, and Antimicrobial Products



Single use (disposable) products help prevent cross-contamination between patients. Products that are designed to be disposable or single use or products that you can designate as patient-specific can help prevent the spread of COVID-19.
Possible single use products include:
|
|
|
Wipe clean and washable products can also be cleaned and disinfected to help with infection prevention. One unique product is the CleanPatch-V, it repairs damaged vinyl furniture so it can be properly disinfected with hospital-grade disinfectants.
Several therapy and medical products can be wiped with disinfectant or washed including:
|
|
Antimicrobial products kill or slow the spread of microorganisms including bacteria, viruses, protozoans, and fungi (like mold and mildew). Other products are bacteria-resistant.
Consider whether it makes sense to incorporate products like these in your clinic or hospital:
|
|
|
How Will You Handle COVID-19 Exposures?
One major consideration for all facilities is what will you do if your staff or patients are exposed to someone who tests positive for COVID-19? If you have an Occupational Health partner, you can work with them to determine exposure policies and procedures.
Be sure to consider questions such as:
- What would be considered an exposure?
- How will you disclose an exposure to patients?
- Will you be able to offer tests to all exposed patients and staff?
- How will you manage if you don’t have testing capabilities for exposed patients and staff?
- How will you handle cleaning and disinfecting your facility?
- How will you educate your staff on these COVID-19 exposure policies?
The CDC also offers an Interim U.S. Guidance for Risk Assessment and Work Restrictions for Healthcare Personnel with Potential Exposure to COVID-19.
COVID-19 Infection Prevention Summary

You want your patients to feel safe when they come in for appointments and you want your staff to feel safe while working. You don’t want people to be so frightened by COVID-19 that they don’t get care in urgent emergency situations.
There is no curative treatment right now, so it’s vital to go back to basics. Hand washing, masks, and social distancing can help protect patients, therapists, and staff. Have a plan ready to go from day one that includes a process workflow, disinfecting procedures, masking and other prevention measures, and how to handle exposures.
By focusing on infection prevention, you can help reduce the risk of your patients and staff contracting COVID-19.
Learn More About Infection Prevention

- Watch this webinar on clinical infection prevention by Lorri Downs, BSN, MS, RN, CIC. She’s a healthcare leader and nurse epidemiologist with experience in infection prevention, surveillance, and clinical informatics who currently works as an infection preventionist at Vanderbilt University Medical Center.
- Read this article on Hospital Acquired Infections (HAI): Prevention Tips & Products for six common HAIs (CLABSI, CAUTI, SSI for colon surgery, SSI for abdominal hysterectomy, CDI, and MRSA).
- Explore the CDC’s Infection Control Guidance for Healthcare Professionals about Coronavirus (COVID-19).
- Check out other infection prevention products!
References
- The New York Times (August 2020). Coronavirus in the U.S.: Latest Map and Case Count. The New York Times. Retrieved from https://nyti.ms/2CAKffO
- CDC. (July 2020). Coronavirus Disease 2019 (COVID-19) Frequently Asked Questions. Centers For Disease Control and Prevention. Retrieved from https://bit.ly/307EK0h
- CDC. (May 2020). Symptoms of Coronavirus. Centers For Disease Control and Prevention. Retrieved from https://bit.ly/2CC2Gkd
- CDC. (July 2020). Coronavirus Disease 2019 (COVID-19) General Business Frequently Asked Questions. Centers For Disease Control and Prevention. Retrieved from https://bit.ly/32i5sGo
- CDC. (April 2020). How to Protect Yourself & Others. Centers For Disease Control and Prevention. Retrieved from https://bit.ly/32iVG6O
- CDC. (May 2020). Hand Hygiene Recommendations. Centers For Disease Control and Prevention. Retrieved from https://bit.ly/2ZqTdFp
- National Pesticide Information Center. (n.d.). Antimicrobials Topic Fact Sheet. Retrieved from https://bit.ly/32gHKtT
- Downs, L. (2020). Infection Prevention: Keep Staff & Patients Safe in a Rehab Clinic. Performance Health Webinar. Retrieved from https://bit.ly/3eurNTk
Medical Disclaimer: The information provided on this site, including text, graphics, images and other material, are for informational purposes only and are not intended to substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other healthcare professional with any questions or concerns you may have regarding your condition.








 France
France Australia
Australia






